Abstract
Background Ischemic and hemorrhagic strokes are common in adults and children with sickle cell disease (SCD). The Cooperative Study of Sickle Cell Disease (CSSCD) estimated that without intervention, 11% and 24% of patients with sickle cell anemia will suffer a stroke by the age of 20 and 45, respectively. The Stroke Prevention in Sickle Cell Anemia (STOP) trial in high-risk children with sickle cell anemia showed a 91% decrease in risk of ischemic stroke for patients randomized to transfusion compared to children managed with standard of care alone. Previous studies showed decreased prevalence of stroke in children with SCD after publication of the STOP trial, suggesting implementation of recommendations from that report. Using statewide hospitalization and emergency department (ED) data from the California Department of Health Care Access and Innovation (HCAI), we determined the cumulative incidence and incidence rates of ischemic stroke, intracranial hemorrhage (ICH), and transient ischemic attacks (TIA) in people with SCD pre- and post-publication of STOP (1998). In contrast to previous investigators who used estimates of SCD prevalence to determine rates, we used a longitudinal cohort.
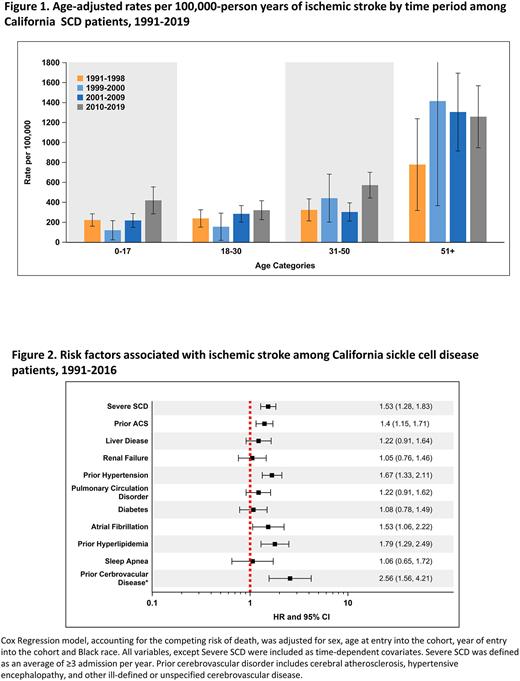
Methods People of all ages with SCD were identified from HCAI data using a previously published algorithm. ICD-9/10 -CM codes were used to identify hospitalizations and/or ED visits for ischemic and hemorrhagic strokes, and TIAs. Age-specific incidence rates per 100,000 person-years across three decades were calculated. To compare to prior reports that showed declining stroke rates in children (<20 years of age) in the two years following publication of STOP using the same data source, age-specific incidence rates for years 1999-2000 were also calculated. Cox proportional hazard regression models, accounting for the competing risk of death, were used to identify risk factors associated with ischemic stroke and ICH. Clinical risk factors were included as time dependent covariates.
Results There were 7,636 patients (53.3% female) of which 548 (7.2%), 227 (3.0%), and 205 (2.7%) presented with a first ischemic stroke, ICH, or TIA, respectively. The cumulative incidences of ischemic stroke, ICH, and TIA were 2.4%, 0.6%, 0.8%, by age 20 and 6.0%, 2.3%, and 2.5%, by the age 40 years, respectively. Figure 1 shows age-specific incidence rates of ischemic strokes over three decades as well as incidence rates two years post-STOP. When compared to prior decades, incidence rates of ischemic stroke increased from 2010-2019 in patients <18 (420) and 31-50 (572) years. In SCD patients <18, there was an initial decrease in the incidence of ischemic stroke two years after STOP. The incidence of ICH increased in patients <18 from 2010-2019 (89) compared to the pre-STOP decade (54). Rates of TIAs increased in patients ³18 in 2010-2019 compared to 1991-1998. In Cox models, hypertension, hyperlipidemia, atrial fibrillation, acute chest syndrome, and severe SCD were associated with increased risk of ischemic stroke (Figure 2). Hypertension, renal failure, Moya Moya, and prior ischemic stroke were associated with increased risk of ICH.
Discussion The incidence of ischemic stroke, ICH, and TIA across age groups were unchanged or increased over the last three decades in Californians with SCD. Compared to results from the CSSCD, our study showed lower cumulative incidences of stroke at 20 and 40 years, which may be due to improved overall SCD care or the CSSCD cohort having a higher disease severity. Using the same California data source as previous investigators, our study also showed a brief decline in ischemic stroke in children after publication of STOP. However, this was followed by an increased incidence of stroke, suggesting that implementation of primary stroke prevention strategies for children were not widely adopted and/or not effective in the real-world setting. Increased sensitivity of imaging used to detect strokes might also have contributed to increased incidence. Incidence of stroke and TIA markedly increased with age, and traditional risk factors were associated with higher risk. These results highlight the need for studies on stroke prevention strategies in adults with SCD that focus on management of hypertension, hyperlipidemia, and other modifiable cerebrovascular risk factors proven effective in the general population and based on robust implementation science.
Disclosures
Keegan:GRAIL: Other: Cancer Survivorship Advisory Board Meeting. Fertrin:Sanofi Genzyme: Consultancy; Global Blood Therapeutics: Consultancy, Speakers Bureau; Agios Pharmaceuticals: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau. Wun:GBT, Inc.: Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal